- Apply
- Visit
- Request Info
- Give
Faculty researchers examine healthcare quandary
Pakdil, Muchiri investigate hospital length of stay versus readmission
Written by Noel Teter '24
Published on January 12, 2026
 Business administration Professor Fatma Pakdil and economics and finance Professor Steve Muchiri have forged an enduring research partnership. Since 2016, the pair has co-authored a series of papers intended to influence healthcare policy.
Business administration Professor Fatma Pakdil and economics and finance Professor Steve Muchiri have forged an enduring research partnership. Since 2016, the pair has co-authored a series of papers intended to influence healthcare policy.
The bulk of their work concerns hospital length of stay (LOS) and readmission rates for patients with serious conditions such as congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD), with implications for patient admission/discharge processes and associated healthcare costs.
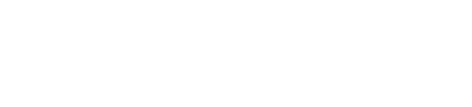
The pair has published several papers concerning Medicare and Medicaid patients in the “International Journal of Healthcare Management.” In a 2024 paper examining LOS and readmission rates in COPD patients, “longer LOS was associated with reduced readmission rates,” said Pakdil. In other words, patients who are able to stay at the hospital longer during their initial stay are less likely to return for the same issue.
Pakdil continued: “In this particular paper, we also found that insurance type, socioeconomic factors including social determinants of health, and hospital characteristics are the factors affecting readmission rates and LOS among COPD patients. So, we have to emphasize the importance of social determinants of health and personalized medicine.”

A common social determinant of health is income level, which influences the quality of insurance patients have and the care they receive as a result. Muchiri explained that lower-income patients are more susceptible to adverse health effects: “If you don't have good health to begin with or you're from a poor home, you're more likely to have more conditions the older you get.”
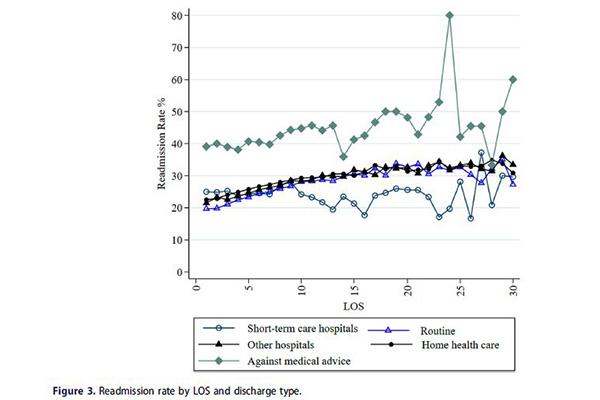
In addition, quality of care metrics, such as optimal expected LOS, can lead to patients being discharged too early, only to be readmitted later. Using a five-day optimal LOS as an example, Muchiri explained, “If you stay more than five days, the insurance is not going to pay for it. If the patient stays less than five days, the hospital gets a profit because it gets paid for five days even though the patient stayed for three,” for example.
He continued: “(Hospitals) are more likely to push for a shorter length of stay because if (patients) stay longer, the hospital doesn’t get paid." However, "if a patient is readmitted, (the patient is) more likely to be penalized (by insurance) for that. If they stay less, they're more likely to be readmitted.”
In other words, readmission results in patients being penalized by their insurance. While hospitals push for lower initial LOS so they may make a profit, patients who do not stay long enough initially are more likely to be readmitted and pay a high price.
Pakdil added: “Once you discharge the patient, you never know when they are going to come back to your hospital. This is a billion-dollar problem for the United States healthcare system.” According to research cited by Pakdil and Muchiri in their 2024 paper, unplanned hospital readmissions presented a $17.4 billion cost to Medicare in 2004.
With patients and hospitals caught between a rock and a hard place, Pakdil and Muchiri hope their research will help policymakers “incentivize better quality of care,” said Muchiri.
Pakdil sees a potential solution in the Hospital Readmissions Reduction Program (HRRP), managed by the Centers for Medicare & Medicaid Services (CMS). “Our findings should be able to help policymakers identify expected LOS for some specific conditions that are monitored by the HRRP,” she said.
Pakdil continued: “Policymakers need to look at the relationship between LOS and readmission. CMS determines the expected LOS for many different conditions. ... From an optimization perspective, what happens to readmission probability if you increase LOS one day or if you decrease LOS one day?”
An enduring partnership
Pakdil and Muchiri’s research partnership began shortly into Muchiri’s tenure at Eastern, when he sought assistance in his expanding research endeavors. “When I joined Eastern, Fatma was there already. She’s an expert in healthcare operations and efficiency, and I had an interest in healthcare,” he said.
“I wanted to work with somebody who has the same mindset I have in terms of setting goals, publishing, and being student-centered,” Muchiri continued. “I was drawn to the idea of collaborating with her because I wanted somebody who could mentor me and push me. Since then, we've been publishing a lot. We have a very good partnership.”
Pakdil added, “Steve was working on healthcare economics. I said, ‘Why don't we work on the same topic together?’ A two-researcher team will be much more effective; if I don't see some aspects, Steve might be seeing that kind of aspect based on his healthcare economics background.”