- Apply
- Visit
- Request Info
- Give
Experts on opioid epidemic open community dialogue at Eastern
Veteran EMT shares first-responder insights
Written by Michael Rouleau
Published on March 06, 2024
Early in his career as a paramedic, in the 1990s, Peter Canning responded to a cheerleading accident in which a high school girl broke her back. Two years later, he responded to her again, this time in a car accident, unconscious from a heroin overdose.
After using naloxone to revive her, he asked the young woman why she started using heroin. Sure enough, it was that same cheerleading accident two years prior that left her addicted to pain medicine. When the prescription finally ran out, she turned to illicit drugs to get her fix.
“I used to think people had a character flaw,” said Canning of those who are addicted to drugs. “That was until I got to know their individual stories.”
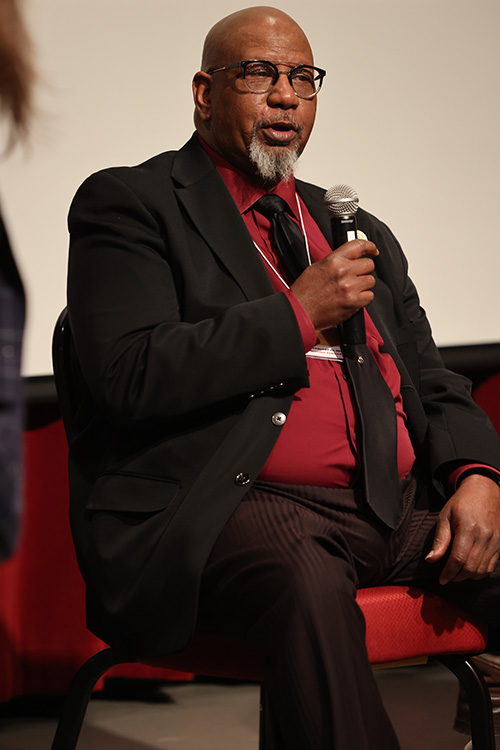
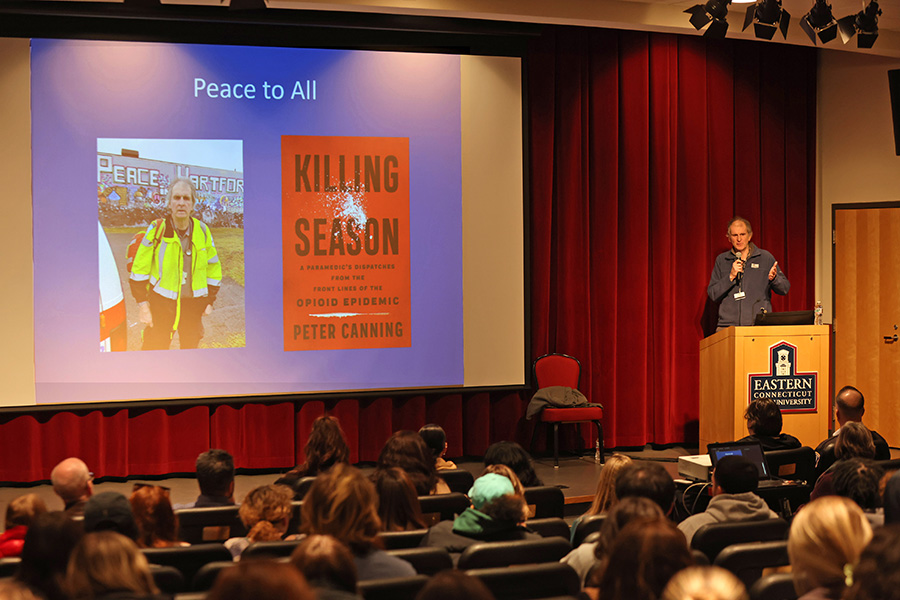
 Canning shared several stories and insights from his 30 years of responding to drug overdoses on Feb. 29 during a symposium at Eastern Connecticut State University focused on finding solutions to the local and national opioid epidemic. A veteran EMT and author of the book “Killing Season: A Paramedics Dispatches from the Front Lines of the Opioid Epidemic,” Canning served as the event’s keynote speaker.
Canning shared several stories and insights from his 30 years of responding to drug overdoses on Feb. 29 during a symposium at Eastern Connecticut State University focused on finding solutions to the local and national opioid epidemic. A veteran EMT and author of the book “Killing Season: A Paramedics Dispatches from the Front Lines of the Opioid Epidemic,” Canning served as the event’s keynote speaker.
Titled “Moving Forward: Community Dialogues on the Opioid Epidemic,” the symposium featured representatives from state and nonprofit agencies, Eastern faculty and community members who have lived with opioid addiction.
The epidemic, which experts say is now in its third wave, started in the ‘90s with prescription painkillers. As prescription pill abuse waned in subsequent years due to tightening regulation, in its place came waves two and three: heroin and, now, fentanyl and the rise of synthetic opioids.
Near the beginning of the epidemic, in 1995, Canning noted that there were approximately 10,000 overdose deaths across the country. In 2016, there were more than 100,000.
Experts agree that the current wave is the most dangerous and deadly. “Fentanyl has totally supplanted heroin in Connecticut,” said Canning, explaining that 90% of heroin in 2017 tested positive for fentanyl, whereas “now, there’s almost no heroin.”
Of the 1,393 overdose deaths in Connecticut in 2023, he said 1,156 were related to fentanyl.
The main problem with fentanyl, according to Canning, is its potency and inconsistent dosage, and the fact that it is often cut with other chemicals. “Fentanyl is 50 times stronger than heroin,” he said. On top of that, its high is short-lived — "it lasts only a couple hours” — requiring users to use it more often. “It’s Russian roulette every time.”
Explaining how addictive opioids are, he said, “The brain becomes hijacked and mistakes (the drug) for a physiological need ... To expect someone with this ‘disease’ to act rationally is like expecting someone with lung disease to climb Mt. Everest.”
That’s how Canning sees addiction: as a disease. “This is not a criminal issue, it’s a public health issue.”
Windham State Attorney Anne Mahoney, who came to Eastern with the idea for the symposium, agreed: “We aren't going to prosecute our way out of this problem ... We need the collective brainpower of the community to address the problem from many angles.”
Recognizing that total abstinence from drug use is not a realistic goal, Canning and others at the event advocated for a harm reduction approach to dealing with the epidemic. Harm reduction aims to minimize damage, utilizing such tactics as needle exchange programs; safe-use sites; and easily accessible community naloxone, an effective medication for reversing overdose.
Several community members who are in recovery identified other barriers to alleviating the epidemic.
Funding long-term treatment was a top priority for the panelists. There are several 30-day programs across the state, but “30 days is too short,” said a panelist named Keith, who has struggled with heroin and fentanyl for 25 years but has been clean for the past five months. “By the time you settle in, it’s over,” and addicts are often pulled back into their old ways, he said.
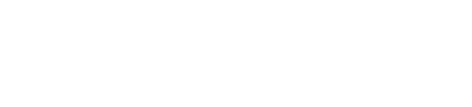
Willimantic Town Councilman Rodney Alexander agreed. “We need to reverse the funding,” he said, by prioritizing treatment over incarceration. Alexander has been sober since 1999. “People need to know that people can and do recover,” he told audience members. “That’s why I’m here.”
Michael Doyle, director of recovery programs at Reliance Health in Norwich, pointed to transportation as an issue. People struggling with addiction are disproportionately homeless or without the means to drive themselves to detox/rehabilitation centers.
To make things more challenging, Stephen Feathers, director of compliance and training at Perception Programs in Willimantic, emphasized that there is a shortage of detox beds. Furthermore, they are first come first serve, he said, so if someone’s able to transport themselves to a center, there’s no guarantee they’ll be treated in time.
Considering how unsteady an addict may be during withdrawal, Feathers noted that there is a “very narrow window to get people into treatment.”
Nancy Navarretta, commissioner of the Connecticut Department of Mental Health and Addiction Services (DMHAS), addressed some of these concerns. DMHAS partners with and administers grants to dozens of providers across the state that are focused on addressing the epidemic.
Thanks to the work of the state’s attorney general office, Navarretta said that Connecticut will receive upwards of $600 million over the next 18 years from settlement payouts related to the opioid crisis. “This funding will go toward evidence-based treatments and harm reduction.”
The symposium was organized by several faculty from Eastern’s social work, health sciences, political science, criminology, sociology and anthropology programs.
“The faculty’s thoughtful planning of the day and their commitment to making meaningful connections with community partners were vital to the success of the event,” said Dean of Arts and Sciences Emily Todd, a symposium organizer. “I was so impressed by the breadth of perspectives we heard from and the high level of engagement, whether from students or members of the community. Many people expressed their excitement about being there, and I think the many different voices participating in the conversation made it especially valuable.”
One of the lead faculty organizers, social work Professor Megan Stanton, added, "Though the opioid epidemic has brought tragedy to so many lives, we also have many people in the community who bring empathy, energy, creativity and commitment to ending this epidemic and supporting people currently impacted by it.”
Other speakers at the symposium included Rebecca Allen, director of recovery advocacy at the Connecticut Community for Addiction Recovery (CCAR); State Senator Saud Anwar; political science Professor Courtney Broscious; Brendan Burke of the Office of the Child Advocate; Noel Casiano, psychology and human services professor at the University of Harford; Lauren Galarneau, clinical director of the Ridge Recovery Center; State Representative Susan Johnson; Avery Lenhart, executive director of the No Freeze Shelter; Eastern Police Chief Stephen Tavares; Jody Terranova, deputy commissioner of the Connecticut Department of Public Health; and more.